In Depth: Wide Complex Tachycardia
Wide complex tachycardia is a cardiac rhythm with more than 100 ventricular beats per minute and a QRS complex of 120 ms or greater. The major clinical problem that arises when dealing with someone exhibiting a wide complex tachycardia is that it is not always immediately clear if the rhythm represents supraventricular tachycardia or ventricular tachycardia. From the learning materials on the ACLS Medical Training site, you may have noticed that the management of supraventricular tachycardia and ventricular tachycardia are different.
Different foci
Four out of five patients with wide complex tachycardia will have ventricular tachycardia. Ventricular tachycardia is, as the name implies, a rhythm that originates in the ventricles. Supraventricular rhythms, on the other hand, originate in the atria and requires atrial input in order to sustain the rhythm. Nonetheless, the ECG tracings of supraventricular and ventricular tachycardia can look similar.
The importance of history
In a patient with wide complex tachycardia, it is much more likely for the person to actually be experiencing ventricular tachycardia if there is a history of structural heart disease or previous myocardial infarction. A patient’s medication list may offer some clues as to the cause of wide complex tachycardia. Drugs such as procainamide and quinidine can increase the risk for ventricular tachycardia. Unfortunately, cardiovascular vital signs are not as useful as one might imagine. Nevertheless, hemodynamic instability is an indication for more aggressive interventions.
A role for physical diagnosis?
Perhaps surprisingly, some patients with ventricular tachycardia are actually hemodynamically stable and may only experience dizziness, palpitations, or no apparent symptoms at all. This means that clinicians cannot rely upon a patient’s vital signs to determine if they are in ventricular tachycardia or not. Despite hemodynamic stability in some patients with ventricular tachycardia, incorrect or untimely diagnosis can be dangerous, if not fatal.
Clues to help diagnosis
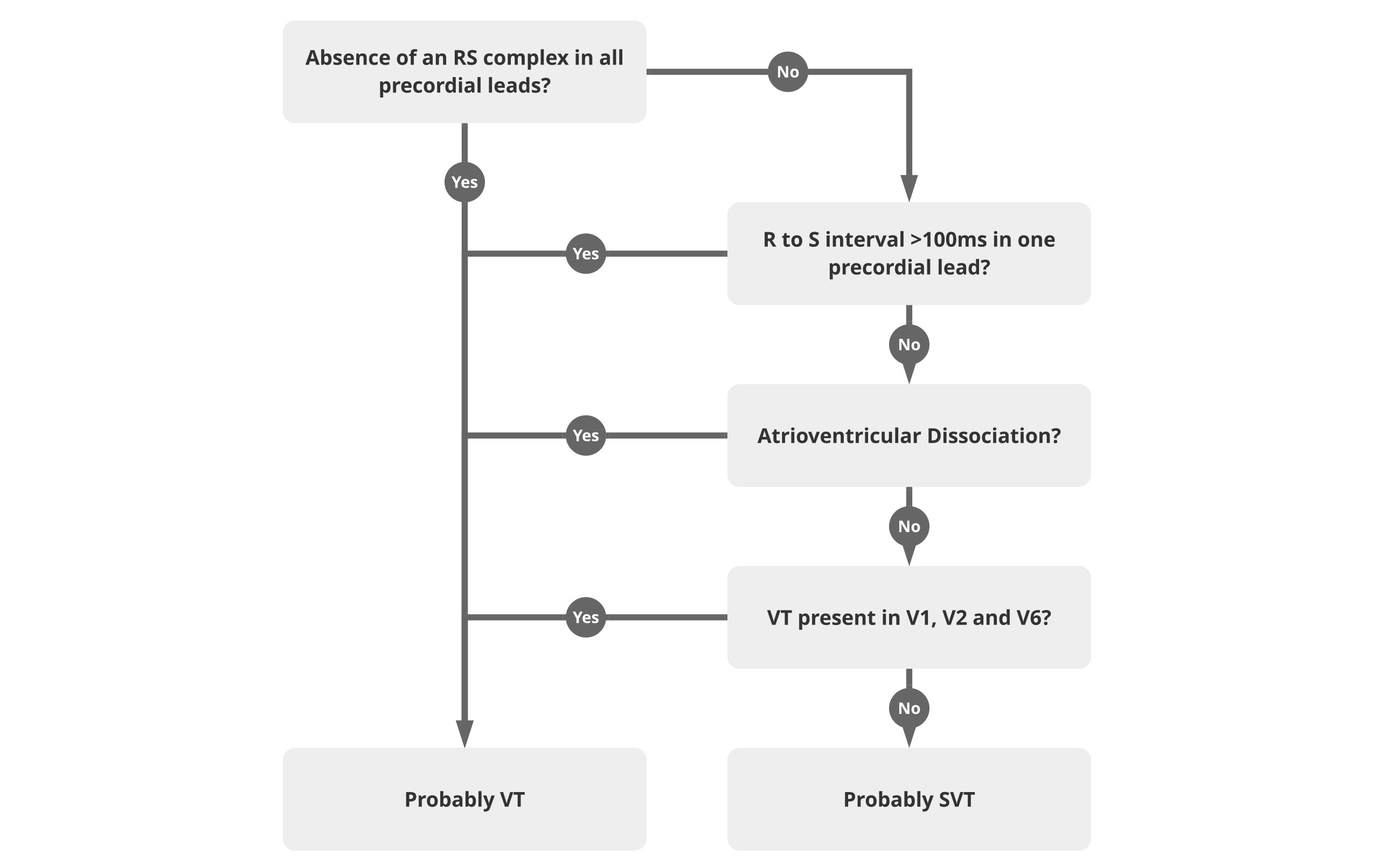
Unfortunately, there is no single diagnostic tool that can be used to definitively differentiate between supraventricular tachycardia and ventricular tachycardia in patients with wide complex tachycardia. One approach that has been developed is called the Brugada algorithm.1 It is a step-by-step process for making a differential diagnosis in wide complex tachycardia.
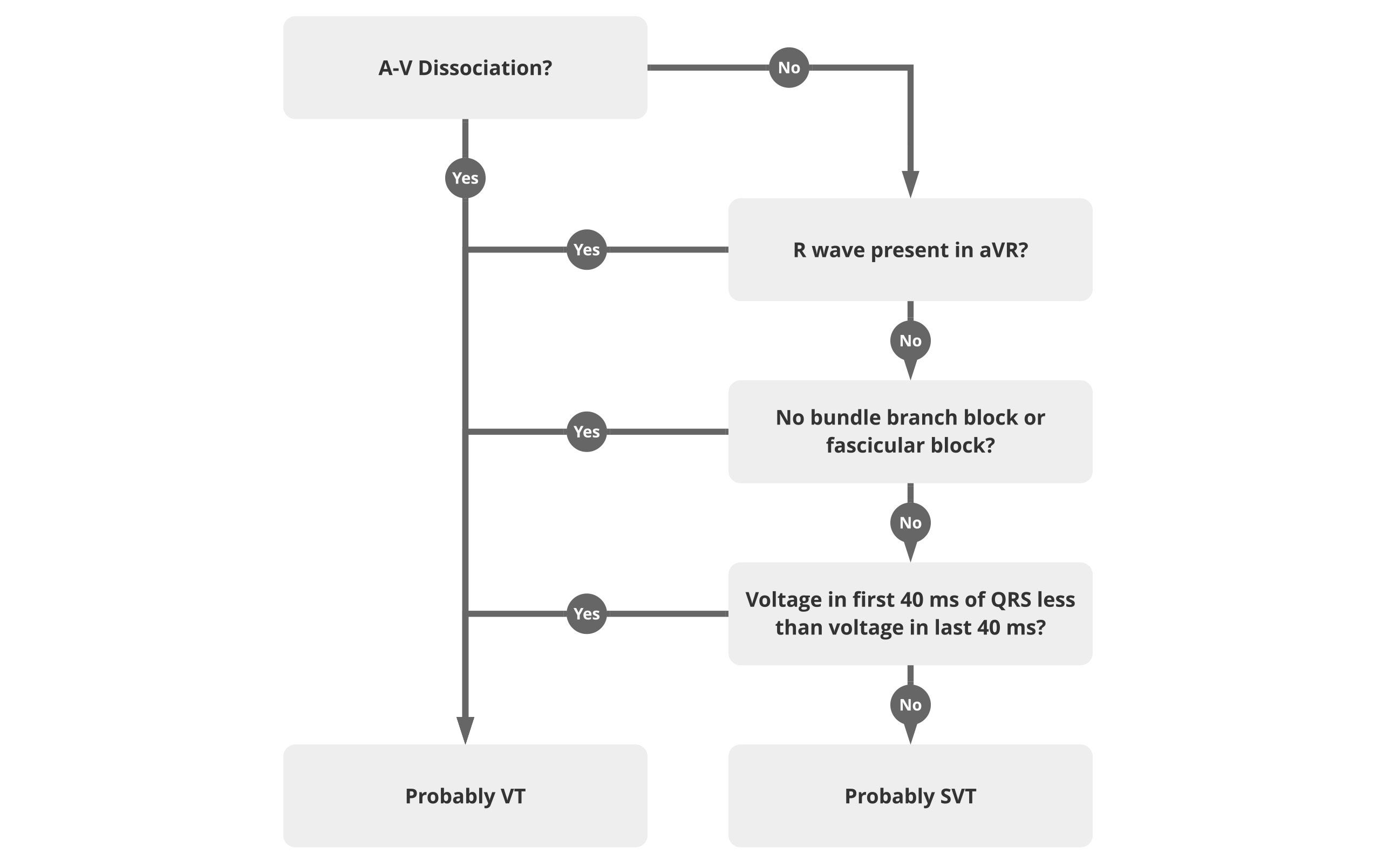
The Brugada algorithm makes sense on paper, but it is a bit unwieldy for use in a clinical situation, especially in an emergent one. A slightly more straightforward rhythm has been proposed.2
Management of an unstable patient
If the patient with wide complex tachycardia is unstable, the differential diagnosis is less important than rapid, decisive action. In most cases, that means applying synchronized cardioversion as soon as possible. If the defibrillator cannot detect a rhythm sufficient to apply synchronized cardioversion, unsynchronized shocks can be given. Also, remember that you will need to provide assistance using ACLS or PALS algorithms.
Management of a stable patient
In a hemodynamically stable patient with wide complex tachycardia, it may be possible to differentiate between ventricular tachycardia and supraventricular tachycardia. In each case, the ACLS algorithm for the respective condition can be followed.
1. Brugada P, Brugada J, Mont L, Smeets J, Andries EW. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. May 1991;83(5):1649-1659.
2. Vereckei A, Duray G, Szenasi G, Altemose GT, Miller JM. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. Eur Heart J. Mar 2007;28(5):589-600.