BLS Suspected Opioid Overdose Algorithm
Opioid overdose can depress a person’s drive to breath and may lead to death. Individuals who are at imminent risk of death from opioids may be given naloxone in pre-hospital settings by trained lay rescuers. Naloxone competes with opioid drugs at opioid receptors, and reverses the effects of the drug. Naloxone has a short half-life in the body—shorter than most opioid drugs of abuse—so multiple administrations may be needed.
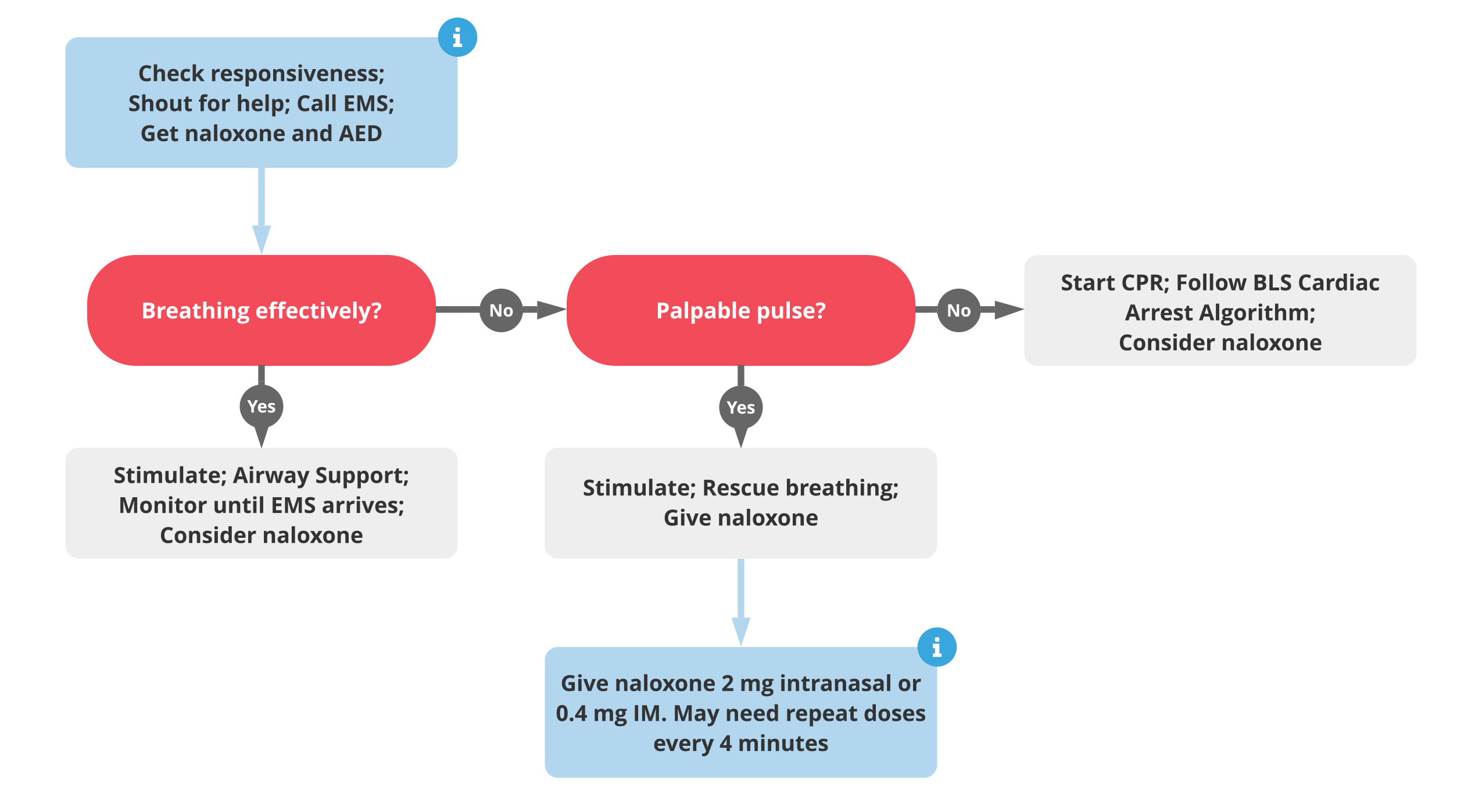
The following algorithm should be followed by rescuers coming to the aid of a person known or strongly suspected to be under the influence of opioid drugs.
- Check for responsiveness. Shake and shout at the victim, if necessary.
- If you are the lone rescuer, use a cell phone to call for help, if one is available.
- If more than one rescuer is available, use a cell phone to call for help, retrieve naloxone and an AED.
- Check breathing and pulse for no more than 10 seconds.
- Perform rescue breathing on victims with a pulse and inadequate breathing. Perform CPR on victims without a pulse and inadequate breathing. If you are the lone rescuer, perform rescue breathing and/or CPR for 2 minutes before leaving the victim to get help and supplies (naloxone, AED).
- Administer naloxone when available. In an out of hospital setting, naloxone can be administered via spray in the nose (2 mg) or with a needle into the arm (0.4 mg). Always follow local dosing and administration protocols.
- If the victim responds, continue to monitor and stimulate the victim (sternal chest rubs, voice commands). If the victim fails to respond or again loses consciousness, resume CPR. You may administer additional doses of naloxone every four minutes.