How to Master Tracheal Intubation
According to the 2000 AHA ACLS Guidelines, tracheal intubation should only be attempted “by healthcare providers experienced in performing this skill”, and expand further by stating that “ALS providers unable to obtain regular field experience… should use alternative, noninvasive techniques for airway management”. This year ILCOR examined evidence to determine if one airway is superior to another in terms of survival and neurologic outcome in cardiac arrest. According to the evidence summary “there is inadequate evidence to show a difference in survival or favorable neurologic outcome”, and recommend that the “choice of bag-mask device versus advanced airway insertion, then, will be determined by the skill and experience of the provider”. The clinician must have sufficient initial and continuing education for whatever airway they choose, and must effectively do so while limiting interruptions in quality CPR.
Some EMS services have demonstrated a 99% success rate for endotracheal intubation, but they probably make up a very small percentage of EMS providers that achieve such proficiency. So why do so many people struggle? The cause of difficulty with skill acquisition is multifactorial, but anecdotally, what I have found from interviewing many students is that their initial education was full of dogma that inevitably left them unprepared to manage difficult airways.
I started my personal airway endeavor with mixed results. When I did successfully place the tube in the trachea, it was usually after several attempts, sweaty palms, and multiple prayers. I thought I knew what I was doing, but had no clue. Once I placed the blade in the mouth, I found structures yet to be defined. So, I took advice from everyone, and was always given different pointers, but nothing worked. Eventually I came to terms with my meager ability to intubate. I accepted the fact that I sucked at laryngoscopy, and the patient would benefit from a supraglottic airway instead of my repeatedly damaging attempts.
Then, at some point I started browsing different blogs, videos, and articles. What I found was that almost all of the airway experts recommend the same basic approach and technique, and nearly all of what others suggested was wrong! I don’t claim to be an expert, but now I approach the airway with confidence knowing what I’m doing is right. I no longer blindly insert the blade only to find unrecognizable tissue, but can actually identify crucial landmarks.
What is the best blade size?
What not to do: Use a Mac 4 on everyone. If the blade is too long, simply back out.
What you should do: While sometimes appropriate, a Mac 4 is not always the best choice for every patient. Novices tend to advance too far, bypassing critical landmarks in the process. A Mac 3 blade is typically long enough for a large majority of adults. A Mac 3 also allows you to lift the tongue and mandible with LESS force than a Mac 4. This video demonstrates the “mechanical disadvantage” of a longer blade.
How do I position the patient?
What not to do: Hyperextend the neck
What some people consider this sniffing position is neck and head extension. I’ve witnessed some people pulling the patient up to the head of the stretcher and letting the head to drop off the edge. This makes the airway more anterior, and intubation more difficult. Dr. Scott Weingart calls this the “bad sniffing position”.
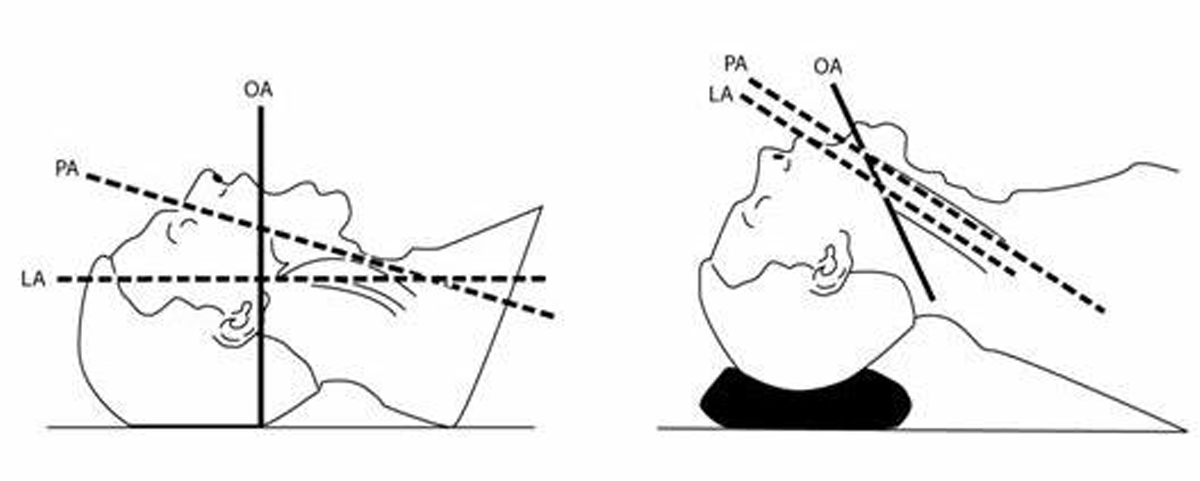
What you should do: Place the patient in the Ear-to-Sternal-Notch position with the face plane parallel to the ceiling.
In this position there is flexion of the neck, and extension of the head (figure 1). The laryngeal axis, pharyngeal axis, and mouth are appropriately in line with the operator’s vision (figure 2). To obtain this position, simply elevate or “ramp” the shoulders and head until the ear-hole is in line with the sternal notch (ramping is particularly useful in obese patients). Position the face on a horizontal plane. This is easily achieved with blankets, pillows, or a combination of both and raising the head of the stretcher.

Figure 1: Copyrighted by Airway Cam Technologies, Inc. (Source: http://www.airwaycam.com/airway-images-drawings)
How do I shape the stylet?
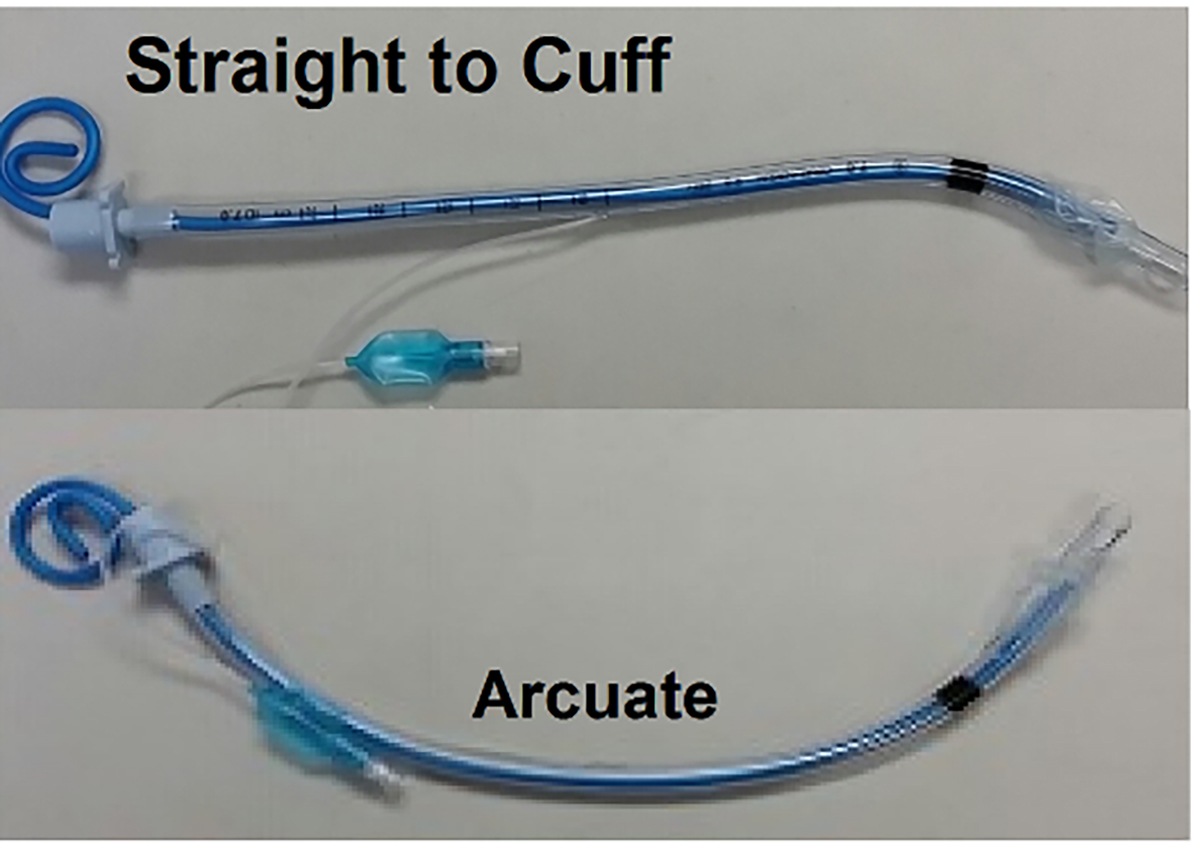
What not to do: Use an arcuate (curved) shape to follow the contour of the tongue.
An arcuate shaped stylet frequently obstructs the line of sight, and can make it difficult to manipulate to tip of the tube towards the pharynx.
What you should do: Instead, shape the stylet and ETT straight to the cuff, and then bend the remaining length at 30-35 degrees—much like a hockey stick (figure 3). This allows you to enter from the right side of the mouth, and easily manipulate the tip of the ETT toward the glottic opening. Dr. Richard Levitan demonstrates why straight-to-cuff shaping is superior.
How do I control the tongue?
What not to do: Insert the blade to the right, and sweep the tongue to the left.
What you should do: As stated before, a common error of most novice clinicians is they miss the landmarks. The most important landmark by far is the epiglottis. Dr. Richard Levitan, known by many as an airway pioneer, said:
“Novice laryngoscopists commonly advance the blade too aggressively, succumb to epiglottis camouflage, and become lost in the pink mucosa of the esophagus with no idea of what they are looking for or how to fix the problem.”
Instead, he recommends inserting the tip of the blade midline, and in very short, methodical movements, slowly advance the blade in a progressive fashion until the edge of the epiglottis is visualized, then gently slide the tip into the vallecular fossa. Dr. Levitan refers to this as epiglottoscopy.
With the tip of tip of the blade properly positioned, the epiglottis can then be lifted via the hyoepiglottic ligament.
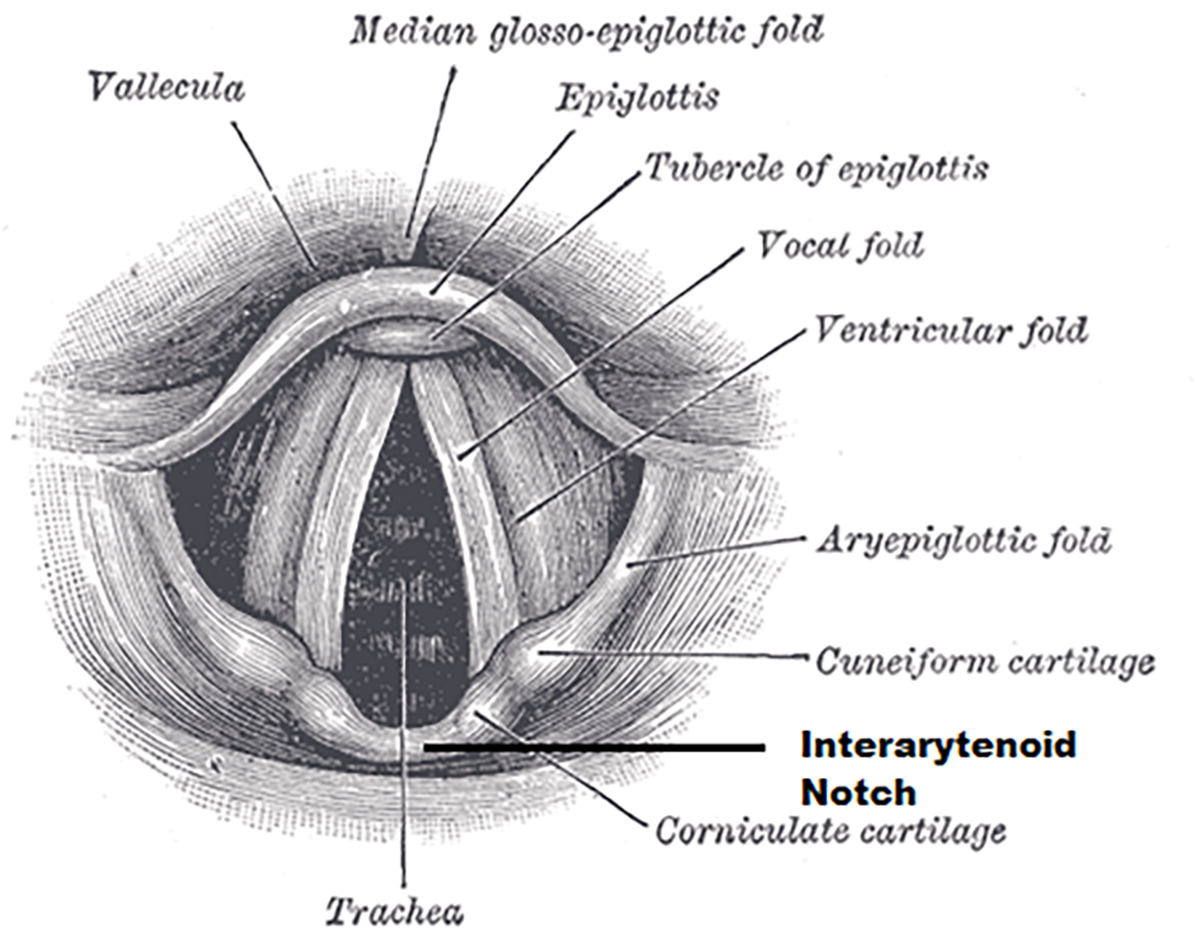
If the epiglottis has been identified, enough force must be applied to successfully lift the epiglottis off the pharynx. Often we’re taught to look for the “vocal cords,” but in reality they may be hidden in darkness and not easily identifiable. The only landmark one has to identify is the interarytenoid notch (Figure 4). Once it’s identified, the ETT can be placed anteriorly into the trachea.
I still don’t have a good view. Now what?
What not to do: Use cricoid pressure to improve your view.
Cricoid pressure does not always compress the esophagus, and can actually displace the larynx making intubation even more difficult. There are more novel methods to improve laryngeal exposure.
What you should do: External Laryngeal Manipulation (ELM) – Also known as bimanual laryngoscopy, ELM involves using the operator’s free hand to manually manipulate the thyroid cartilage. Holding the laryngoscope in the left hand, the operator then reaches around and manipulates the thyroid cartilage with his or her right hand, and moves it back, up, or sided to side to improve the view. Once the structures are visualized, an assistant can take over ELM, and the laryngoscopist can verbally express which way the assistant should manipulate the larynx (Figure3). This is NOT BURP (Backward, upward, rightward pressure) or cricoid pressure.
Head Elevated Laryngoscopy Positioning (HELP) – Maybe counterintuitive to some who “hyper-extend” the neck, elevating the head can result in an improved laryngeal view when compared to the “normal” sniffing position. Hochman et. al. concluded that:
“Increasing head elevation and laryngoscopy angle (neck flexion) significantly improves POGO scores during laryngoscopy on fresh human cadavers.”
Held elevation can be performed by an assistant who elevates the head beyond the ear to sternal notch position and decreases the angle between the patients chin and their chest.
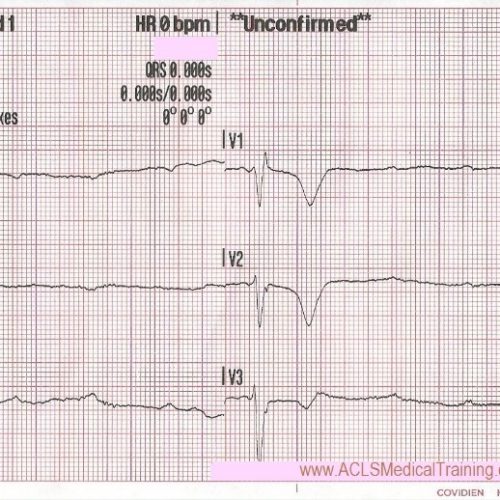
How do I confirm tube placement?
The answer to this question is and should be unequivocally continuous waveform capnography. With a sensitivity and specificity of 100% reported by some studies, initial confirmation as well as continuous monitoring should be performed using waveform capnography. This sensitivity could be less in circumstances such as massive pulmonary embolism, or prolonged cardiac arrest, but these are most certainly rare exceptions. Clinical assessment is still key and should be relied on to ensure placement is not in the right main stem.
In summary:
- Preparation
a. Select the right blade size.
b. Shape the stylet and ETT straight to the cuff, then bend at a 30-35 degree angle.
c. Properly position the patient Ear-to-Sternal-Notch with face plane parallel to ceiling. - Epiglottoscopy
a. Progressively and methodically advance the tip of the blade midline and gently seat in the vallecula. - Laryngeal Exposure
a. If the view is still not optimal, consider trying ELM, or HELP to improve visualization. - Tube Delivery
a. Using straight-to-cuff shaping, insert near the right corner of the mouth and advance upward.
b. Pass the tip anterior to the interarytenoid notch.
c. Ensure the cuff of the tracheal tube is below the level of the cords. - Tube Confirmation and Maintenance
a. Direct visualization
b. Absent sounds over the epigastrium
c. Equal bilateral breath sounds
d. Good compliance with the BVM
e. Tube fogging (never primary)
f. Continuous waveform capnography (for confirmation and maintenance)
g. Rising SpO2 (for patients with a pulse)
References
http://www.ncbi.nlm.nih.gov/pubmed/12605198
King County 2013 Annual Report. Weblog post. Kingcounty.gov. N.p., n.d. Web. 7 Nov. 2015.
Levitan, Richard M. The Airway Cam Guide to Intubation & Practical Emergency Airway Management. Wayne, PA: Airway Cam Technologies, 2004. Print.
Levitan, Richard. “Head Elevated Laryngoscopy Position.” H Ead-Elevated Laryngoscopy Position: Improving Laryngeal Exposure During Laryngoscopy by Increasing Head Elevation (n.d.): n. pag. Web. 8 Nov. 2015.
Nickson, Chris. “ETT Stylet | LITFL: Life in the Fast Lane Medical Blog.” LITFL Life in the Fast Lane Medical Blog. N.p., n.d. Web. 08 Nov. 2015.
Nickson, Chris. “Cricoid Pressure.” LITFL Life in the Fast Lane Medical Blog. N.p., n.d. Web. 08 Nov. 2015.
Rogers, Joe. “NOVEL TIPS FOR AIRWAY MANAGEMENT – Emdocs.” Emdocs. N.p., 30 Dec. 2014. Web. 08 Nov. 2015.


Comments