ACLS Bradycardia Algorithm
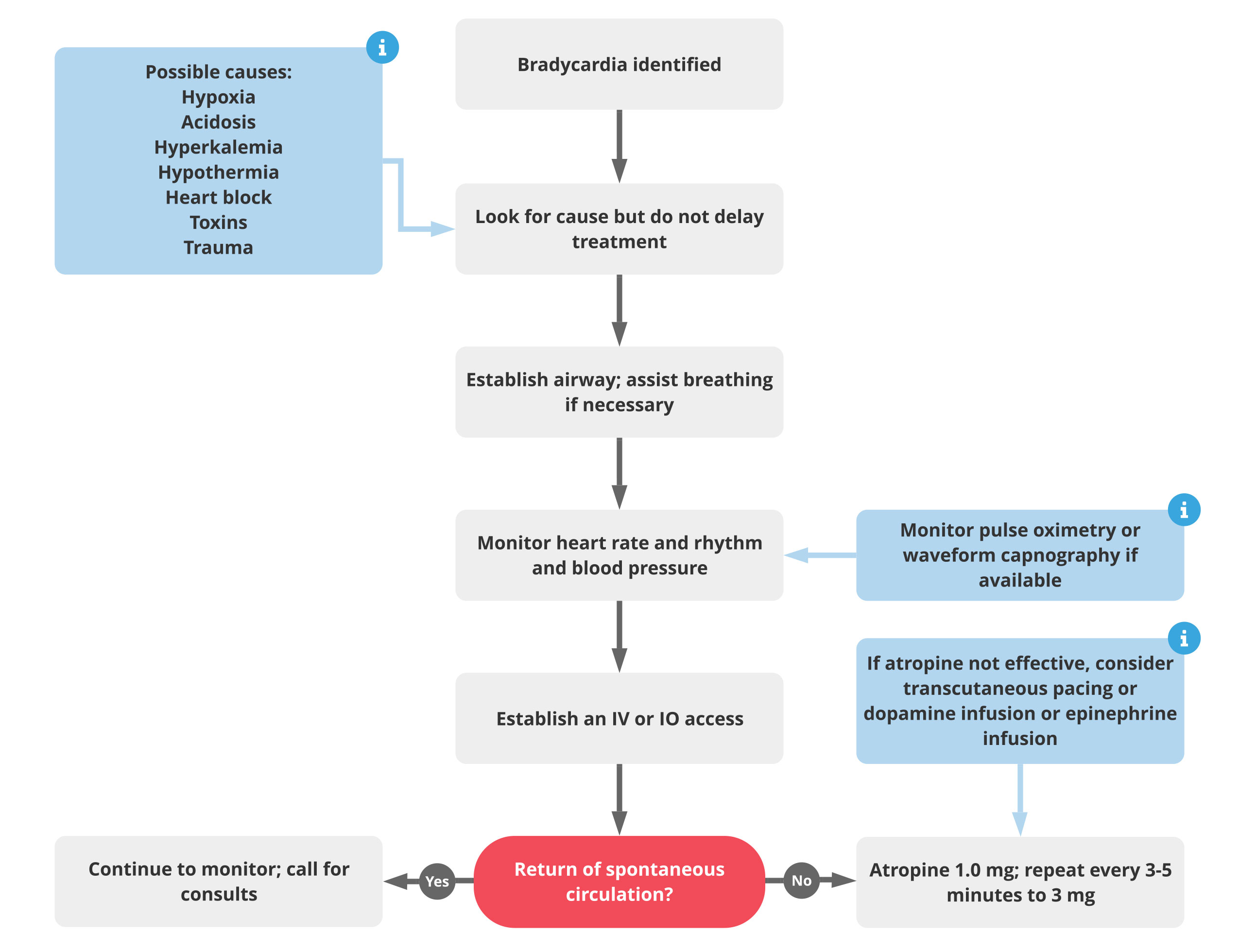
Treatment for bradycardia should be based on controlling the symptoms and identifying the cause using the Hs and Ts
- Do not delay treatment but look for underlying causes of the bradycardia using the Hs and Ts.
- Maintain the airway and monitor cardiac rhythm, blood pressure and oxygen saturation.
- Insert an IV or IO for medications.
- If the patient is stable, call for consults.
- If the patient is symptomatic, administer atropine 1.0 mg IV or IO bolus and repeat the atropine every 3 to 5 minutes to a total dose of 3 mg:
- If atropine does not relieve the bradycardia, continue evaluating the patient to determine the underlying cause and consider transcutaneous pacing
- Consider an IV/IO dopamine infusion at 2-10 mcg/kg/minute
- Consider an IV/IO epinephrine infusion at 2-10 mcg/minute.
- In the cases of Mobitz type II second-degree heart block, third-degree AV block, or third-degree AV block with new widened QRS complex, atropine is unlikely to be effective. Consider transcutaneous pacing immediately or a beta-adrenergic infusion to increase heart rate.
The Hs and Ts of Bradycardia
| Potential Cause | How to Identify | Treatments |
| Hypovolemia | Rapid heart rate and narrow QRS on ECG; other symptoms of low volume | Infusion of normal saline or Ringer’s lactate |
| Hypoxia | Slow heart rate | Airway management and effective oxygenation |
| Hydrogen Ion Excess (Acidosis) | Low amplitude QRS on the ECG | Hyperventilation; consider sodium bicarbonate bolus |
| Hypoglycemia | Bedside glucose testing | IV bolus of dextrose |
| Hypokalemia | Flat T waves and appearance of a U wave on the ECG | IV Magnesium infusion |
| Hyperkalemia | Peaked T waves and wide QRS complex on the ECG | Consider calcium chloride, sodium bicarbonate, and an insulin and glucose protocol |
| Hypothermia | Typically preceded by exposure to a cold environment | Gradual rewarming |
| Tension Pneumothorax | Slow heart rate and narrow QRS complexes on the ECG; difficulty breathing | Thoracostomy or needle decompression |
| Tamponade – Cardiac | Rapid heart rate and narrow QRS complexes on the ECG | Pericardiocentesis |
| Toxins | Typically will be seen as a prolonged QT interval on the ECG; may see neurological symptoms | Based on the specific toxin |
| Thrombosis (pulmonary embolus) | Rapid heart rate with narrow QRS complexes on the ECG | Surgical embolectomy or administration of fibrinolytics |
| Thrombosis (myocardial infarction) | ECG will be abnormal based on the location of the infarction | Dependent on extent and age of MI |